“Ideon does all the heavy lifting—cleansing, filtering, refining all that data from carriers—and then they output a single, consistent data format that’s really easy for us to consume”
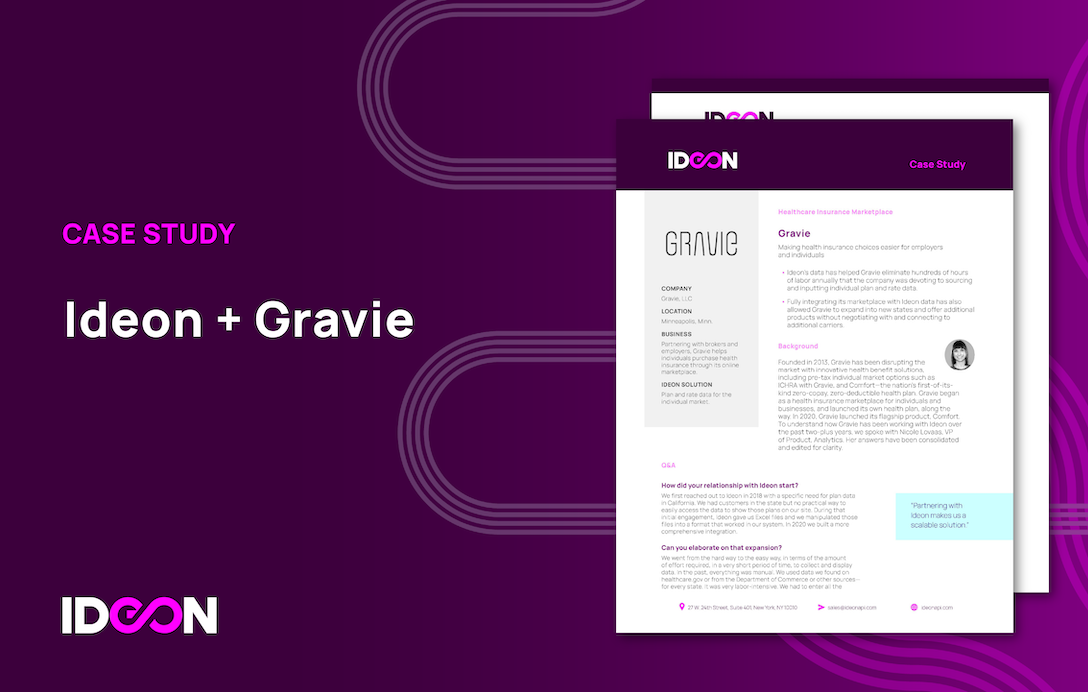
PerfectQuote is a SaaS solution for employee benefits brokers and agents, founded in 2017 on the hypothesis that there had to be an alternative to the manual spreadsheeting of benefits and rates. And indeed there was. With PerfectQuote’s software, benefits brokers in the large group space can now quote, analyze, compare, and present plans from carriers in all 50 states.
But what of the small-group space, you ask?
Powered by Ideon, PerfectQuote now offers one of the industry’s leading small group quoting experiences. Want an inside look at how PerfectQuote expanded its platform? See below.
Perfect Quote
Helping Employee Benefits brokers and their teams sell more, faster and better
- Ideon’s data powers the small-group side of PerfectQuote’s Group Insurance CPQ software.
- Ideon’s data helps PerfectQuote eliminate thousands of hours of labor that would otherwise be devoted to sourcing, normalizing and presenting plan and rate data.
Background
Since 2017, PerfectQuote has provided quoting, analysis and presentation software to group brokers and general agents, with the goal of supporting plans for small (ACA) and large-group medical in all 50 states, alternative-funded and ancillary lines of coverage.
To understand how the company works with Ideon, we spoke with Aaron Snyder, president and co-founder, and Curtis Kadohama, head of product. Their answers have been consolidated and edited for clarity.
Q&A
What’s the cocktail party version of PerfectQuote?
Aaron Snyder: PerfectQuote’s CEO and co-founder, Justin Sylvester, was an employee benefits consultant. Around 2013 he started thinking that there had to be a better way to support brokers and their teams in the manually intensive process of spreadsheeting benefits for clients. He developed the initial push of the idea and in 2017, we started to collaborate. The next year we came out with our first product, called PerfectQuote, with the proposition that we could eliminate the laborious data entry that had been required to sell and renew insurance for brokers in the large group space. While brokers had some options for small group, PerfectQuote was designed to allow brokers to upload any quote file, from any carrier, for any size group. From this point, they would have the ability to analyze and present employee benefits options quickly and easily and without error.
How does Ideon enter into this?
Aaron Snyder: As I mentioned, one of our main differentiators is that we support the large-group portion of a broker’s book of business, with plan and rate data that we get directly from carriers. But on the small-group side, which involves many more carriers, we didn’t have a solution that could support a broker’s entire book of business. So, like any nimble start-up, we developed our small group module and quickly figured out that Ideon could be a single source of truth for small group data,and eliminate some of the friction we experience within the other side of the platform. Ideon provides a very essential function for us.
Why is it such an essential function?
Curtis Kadohama: The easiest way to understand the value of Ideon is to compare our small group and large group data workflows. In the large group market, every carrier has its own format for quote files, each of which may also vary by state. So we’re constantly having to adapt to new file formats, new layouts, new ways of carriers interpreting and illustrating benefit values. It’s highly manual and time intensive. Compare that to our small-group workflow. Ideon does all the heavy lifting—cleansing, filtering, refining all that data from carriers—before they output a single, consistent data format that’s easy for us to consume.
Can you quantify the savings in time or effort from using Ideon as your small-group data source?
Curtis Kadohama: We’ve done some rough analysis. Let’s say there’s a new PDF quote file we receive from one carrier for one state covering one plan. We estimate it would take us 15 hours in terms of scraping, mapping, analyzing, developing, QAing, and refining before we can say, “Okay, it’s ready to use by our brokers.” Now compare that to what happens with Ideon. We’ve already done our integration with them, which took some development time—and each year we’ll spend a little dev time on updates—but for a given employer group, depending on the state, our application could give a broker 700 or 800 plans to present to his or her client, in a matter of seconds. In contrast, a broker’s offering to a client is typically limited to how many spreadsheets of plans can be manually created using carrier documents and PDFs. It’s a pretty drastic difference.
Are there benefits to partnering with Ideon beyond time savings?
Curtis Kadohama: Having a dependable source of data helps on the inbound side, in terms of knowing that we’re receiving reliable information. It allows us to consistently and confidently display information in our application and in our Excel exports to customers. Compare that, again, to our large-group side, where the data we receive is both inconsistent in terms of categorization of information and challenging in terms of quality, with missing decimal places, dollar signs, percentage signs. It’s a difficult experience for everyone, from the people on our team processing that data to the end brokers who have to interpret it. Ideon basically removes those challenges from the small-group side of our business—and to the extent that there are questions or complexity to clarify, which is inevitable, the Ideon team is highly responsive.