NEWARK, N.J. – Prudential Financial, Inc. (NYSE: PRU) announced today that its Group Insurance business has collaborated with Ideon, a leader in data exchange and connectivity solutions, to deliver unique technology solutions for benefits eligibility and enrollment processes for workplace clients and their employees.
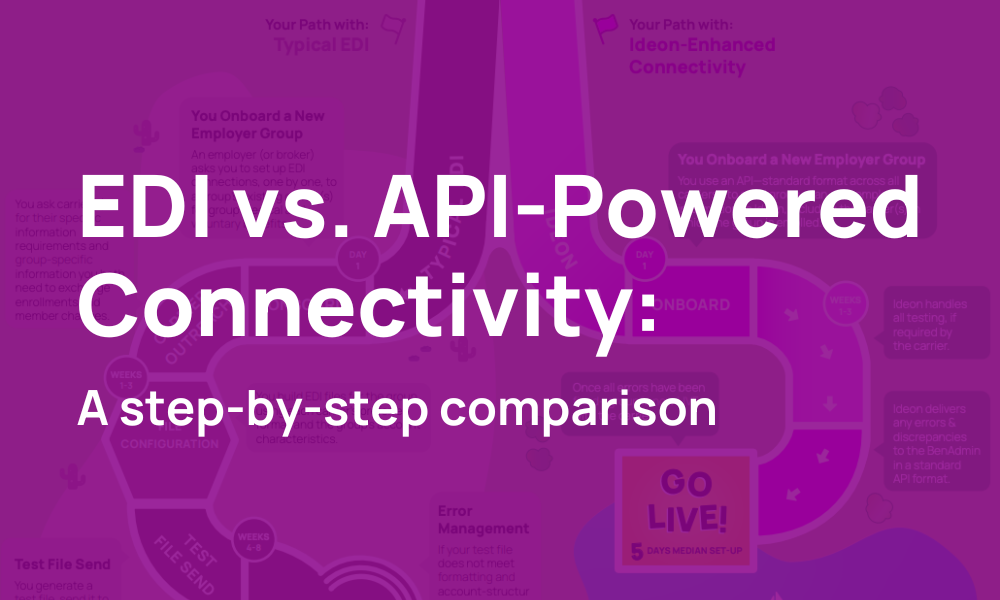
As employers expand their benefits offerings to attract and retain top talent, the need for fast, safe and efficient benefits administration has never been greater, with high expectations around data exchange between providers, employers and the benefit administration systems they use. Through this strategic relationship with Ideon, Prudential aims to improve the accuracy of enrollment data, help reduce the administrative workload for human resources teams, and seek new and innovative ways to ensure accurate enrollment and eligibility data. The collaboration will also allow Prudential to expand integrations with certain benefit administration systems where connectivity is limited today.
“We are committed to providing a superior experience for our clients and their employees,” said Jess Gillespie, head of product and underwriting for Prudential Group Insurance. “Enhancing Prudential’s digital connectivity makes it faster and easier for groups, and their employees, to enroll in workplace benefits.”
The initial phase of the collaboration focuses on expediting the data exchange process that impacts the onboarding process, including enrollment and eligibility information.
“This relationship signifies a major step forward for Ideon and Prudential,” said Steve Swad, CEO of Ideon. “Our data solutions will enable Prudential to deliver a fast, seamless, and accurate benefits enrollment and administration experience. We are excited to support Prudential in enhancing their platform ecosystem.”
For more information, visit Prudential Group Insurance or Ideon.
About Prudential
Prudential Financial, Inc. (NYSE: PRU), a global financial services leader and premier active global investment manager with approximately $1.6 trillion in assets under management as of Sept. 30, 2024, has operations in the United States, Asia, Europe, and Latin America. Prudential’s diverse and talented employees help make lives better and create financial opportunity for more people by expanding access to investing, insurance, and retirement security. Prudential’s iconic Rock symbol has stood for strength, stability, expertise, and innovation for nearly 150 years. For more information, please visit news.prudential.com.
About Prudential Group Insurance
Prudential Group Insurance manufactures and distributes a full range of group life, long-term and short-term disability and corporate and trust-owned life insurance in the U.S. to institutional clients primarily for use within employee and membership benefit plans. The business also sells critical illness, accidental death and dismemberment and other ancillary coverages. In addition, the business provides plan administrative services in connection with its insurance coverages, and administrative services for employee paid and unpaid leave, including FMLA, ADA, and PFL.
About Ideon
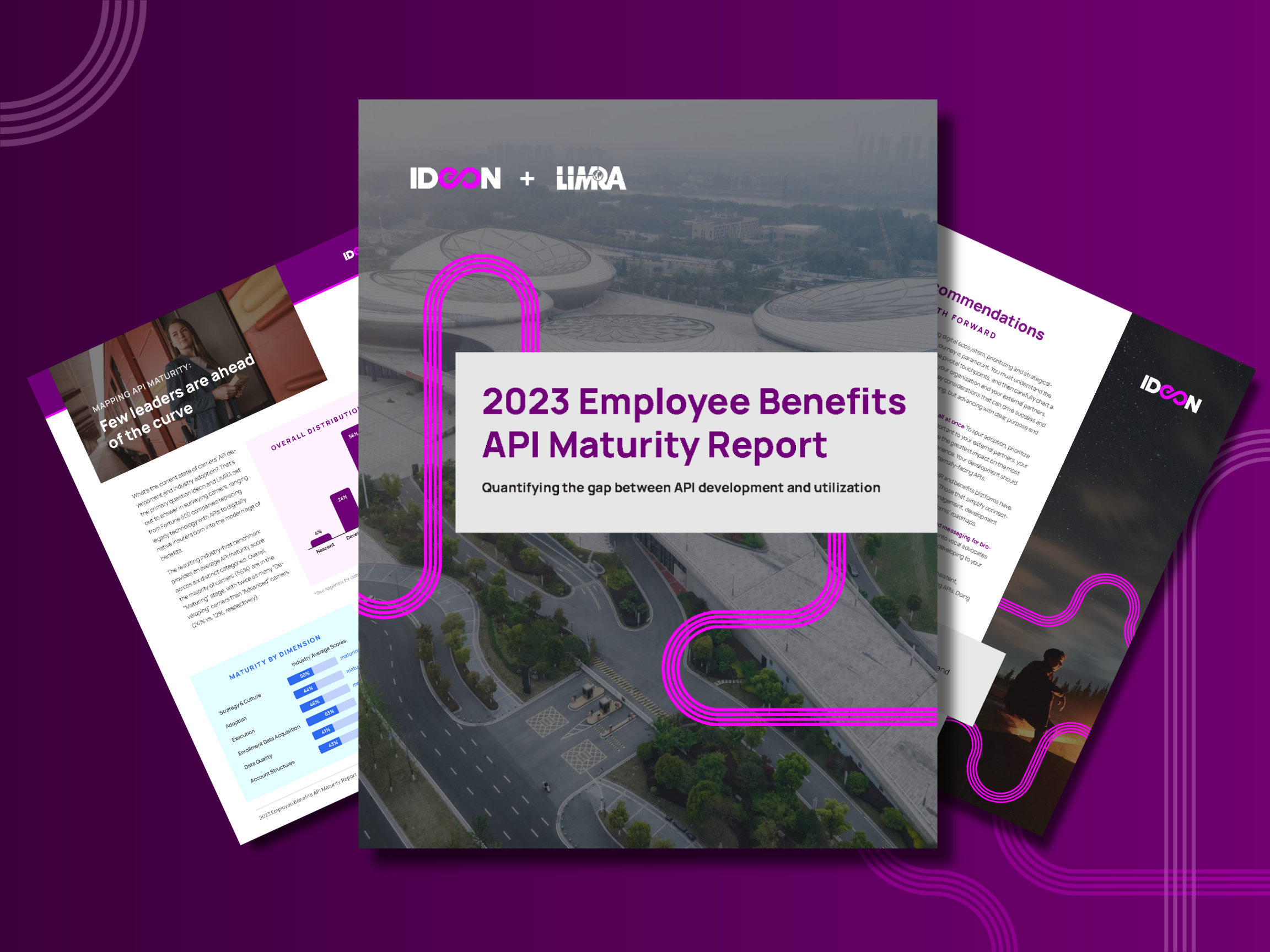
Ideon’s data solutions allow health insurance carriers and employee benefits providers to connect with technology partners to deliver seamless consumer experiences at every stage of the member journey. Ideon serves as the infrastructure simplifying the exchange of quoting, provider, and enrollment data between carriers and the technology partners, so they can deliver health and employee benefits to hundreds of millions of Americans every day. Ideon transmits billions of data points between insurtechs and insurance carriers, powering an amazing benefits experience for all. To learn more, please visit ideonapi.com.