Ideon Blog
May 10, 2018
By: Ideon
VeriStat: How the Top 10 Cost Driving Drugs are Covered in the ACA Market: Part III
**Ideon is the company formerly known as Vericred. Vericred began operating as Ideon on May 18, 2022.**
This is the final post of a three-post series on this subject.
Which prescription drugs do we spend the most money on as a nation, and how are they covered in the ACA market? In this post, we will explore the differences in coverage of certain cost driving drugs between the individual and small group markets.
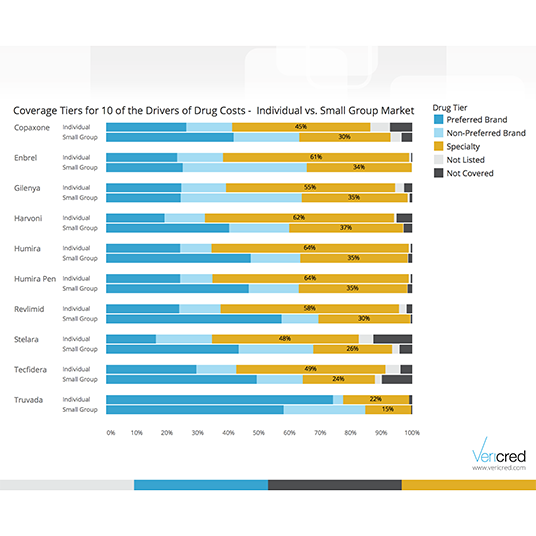
According to the Express Scripts 2016 Drug Trend report, the prescription drugs in the chart below drive significant aggregate cost based on unit cost as well as utilization. The cost of drugs to an employee and his/her family is determined their employer’s health plan’s design and drug formulary. Formularies are lists of prescription drugs with each drug each in a “tier.” Typical plan tiers, from least expensive to most expensive, are as follows: generic, preferred brand, non-preferred brand and specialty.
In prior posts, we looked at coverage analyses of these ten cost-driving drugs in both the individual and small group markets. To do so, we looked at formularies for these ACA health plans across the nation to see how each of these drugs is covered. The results show a significant difference in coverage between individual and small group health plans.
In general, health plans for individuals cover these high cost drugs at higher cost tiers, while small group health plans cover these high cost drugs at lower cost tiers. The difference in coverage between these two markets is meaningful. As small(er) businesses are considering whether they directly offer a health plan or encourage their employees to seek coverage through the individual market, they may want to take into consideration these differences in coverage.

In future posts, we will explore the differences in plan premiums between the individual and group markets.