Ideon Blog
May 03, 2018
By: Ideon
VeriStat: How the Top 10 Cost Driving Drugs are Covered in the ACA Market: Part II
**Ideon is the company formerly known as Vericred. Vericred began operating as Ideon on May 18, 2022.**
This is the second post of a three-post series on this subject.
Which prescription drugs do we spend the most money on as a nation, and how are they covered in the ACA market? In this post, we will explore the coverage of certain cost driving drugs in the small group market.
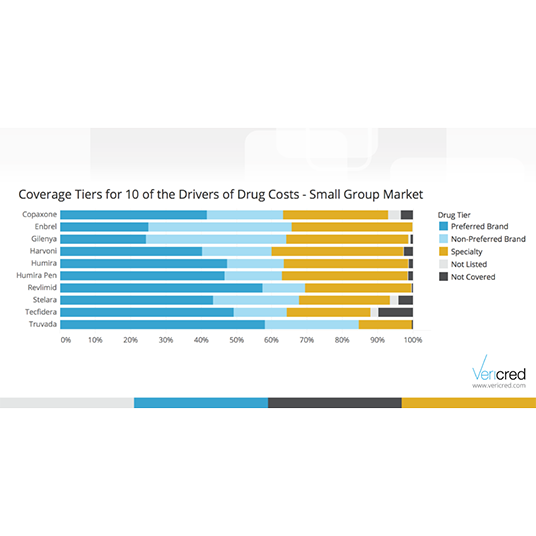
According to the Express Scripts 2016 Drug Trend report, the prescription drugs in the chart below drive significant aggregate cost based on unit cost as well as utilization. The cost of drugs to an employee and his/her family is determined by their employer’s health plan’s design and drug formulary. Formularies are lists of prescription drugs with each drug listed in a “tier.” Typical plan tiers, from least expensive to most expensive, are as follows: generic, preferred brand, non-preferred brand and specialty.
The data science team at Vericred developed a coverage analysis of these ten cost driving drugs in the small group market. We looked at formularies for small group health plans across the nation to see how each of these drugs is covered. The results show that a majority of small group ACA plans cover these drugs in the preferred brand or non-preferred brand tiers, but approximately one third of plans cover these drugs in the specialty tier; the most expensive tier other than not being covered at all. Given the wide variation in coverage, employers may want to consider whether or not their employees and/or dependents are taking these high cost medications when choosing a health plan.