Ideon Blog
May 07, 2019
By: Ideon
Medicare Advantage: What it is, how it works and why the market is growing
**Ideon is the company formerly known as Vericred. Vericred began operating as Ideon on May 18, 2022.**
We’ve made it our mission to enable technology companies to build innovative solutions that bring transparency, efficiency and decision support to the health insurance and employee benefits spaces. Earlier this week we launched our Medicare Advantage Rating API, which will now allow InsurTech and digital health platforms to deliver plan search, quoting and other features to seniors, employers and brokers in the flourishing over-65 market.
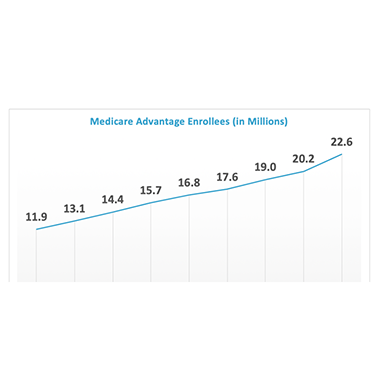
Using Vericred as their data foundation, technology companies including online brokers can use the new API to build Medicare Advantage solutions to better support the 22 million Americans now enrolled in Medicare Advantage plans. Let’s dive in to better understand Medicare Advantage basics and why these plans are increasingly popular.
Medicare Advantage — also known as Medicare Part C — is a privately administrated type of Medicare, which is the United States government’s federal health insurance program for Americans age 65 and older and younger people meeting certain criteria.
Traditional Medicare consists of two parts:
- Part A – Hospital Insurance: Most beneficiaries are eligible for Part A premium-free, which covers inpatient hospital stays, care in a nursing facility and hospice services.
- Part B – Medical Insurance: Part B covers outpatient medical care, such as preventive services, doctors’ visits, laboratory and diagnostic tests, vaccinations and outpatient procedures. The premium for Part B is $135.50 monthly for most people, but those in higher income brackets pay as much as $460.50 per month.
Enacted as part of the Medicare Modernization Act of 2003, Part D adds coverage for self-administered prescription drugs. Part D plans can be purchased to supplement Original Medicare (Parts A and B) or bundled into a Medicare Advantage Plan.
What is Medicare Advantage (Medicare Part C)?
Medicare Advantage is a program in which individuals who qualify for Medicare can enroll in alternative, certified health plans offered by private insurance companies instead of the government-run Original Medicare plan (Part A + Part B). These plans include Part A, Part B, and usually Part D.
What services do Medicare Advantage plans cover?
Medicare Advantage plans are regulated by the Centers for Medicare and Medicaid Services (CMS) and must cover all of the services — except hospice — that Medicare Parts A and B cover. In addition, many Medicare Advantage plans also cover benefits not included in Original Medicare, such as vision, hearing and dental coverage, in-home support, wellness programs, and other supplemental services.
How does Medicare Advantage work?
The U.S. government (Medicare) pays the private insurance carrier offering the Medicare Advantage plan a fixed monthly fee for each enrolled member. Members are then provided coverage through the private carrier rather than through the government. Unlike with Original Medicare, which permits members to visit any healthcare provider who accepts Medicare, Medicare Advantage enrollees may be limited only to doctors, specialists and hospitals within their private insurance carrier’s provider network.
How much do enrollees pay?
Most Medicare Advantage beneficiaries pay monthly premiums to their private insurance carrier that vary depending on the specific plan in which they’re enrolled. These premiums can range from just a few dollars to hundreds of dollars per month. Some “zero premium” plans do not require members to pay a separate Medicare Advantage premium at all, but nevertheless these plans are not free, as enrollees must continue to pay the $135.50 (or more) Part B premium. Some Medicare Advantage plans go even further and pay some or all of the Part B premium, reducing the amount the beneficiary pays to the government each month for Medicare coverage. According to CMS, the average monthly Medicare Advantage premium (not including Part B) is $28, a six percent decrease compared with 2018.
In addition to premiums, beneficiaries are also responsible for paying a portion of the healthcare costs they incur. Under Original Medicare, enrollees are responsible for paying 20% of the costs of most services and have no out-of-pocket limit. Medicare Advantage plans, however, often charge members a set dollar amount — instead of a fixed percent — for most services and have an annual out-of-pocket maximum, after which the insurance carrier will pay for all covered costs.
Why is Medicare Advantage becoming more popular?
By providing supplemental, flexible benefits, and low premiums, Medicare Advantage plans have proven attractive to Medicare enrollees. According to CMS, the number of Medicare Advantage enrollees nationwide has expanded this year to an all-time high of about 22 million, a 32 percent increase since 2015. This represents about 36 percent of all Medicare beneficiaries.

Up Next: VeriStat series on Medicare Advantage plans and benefits
As we’ve explored above, Medicare Advantage is an expanding, popular and diverse alternative to Original Medicare, albeit with a different cost-sharing structure and wide-ranging benefits. Next, our VeriStat series jumps into deeper analysis to further investigate the intricate Medicare Advantage market and its various plan designs.
Interested in building digital user experiences for the Medicare Advantage market? Check out Vericred’s digital toolkit, which includes use cases on developing solutions for this growing insurance market.